Results
- Results of Wave 1 of the modified Delphi process are presented in this poster
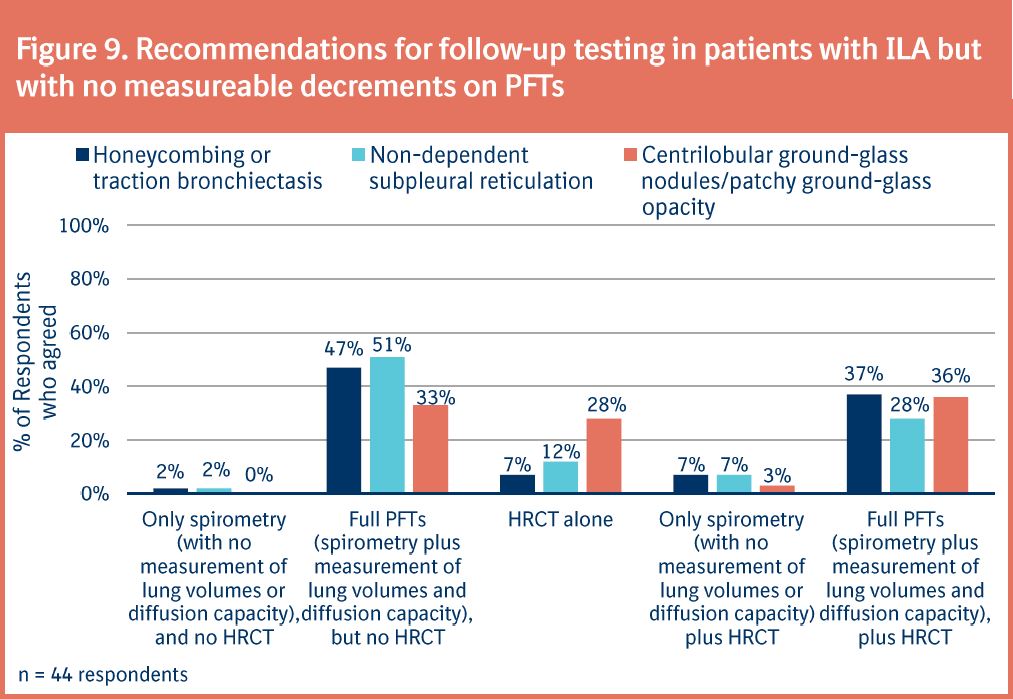
- Pulmonologists and radiologists constituted approximately three-quarters and one-quarter of the expert panel, respectively (Figure 2)
- Most members practiced within academic centers or teaching hospitals (Figure 2)
- Expert panel members (n = 44) were experienced clinicians, 59% of whom had >15 years of experience
- Members had extensive ILD specialization; 52% had treated >200 patients with ILD in the previous year
Image
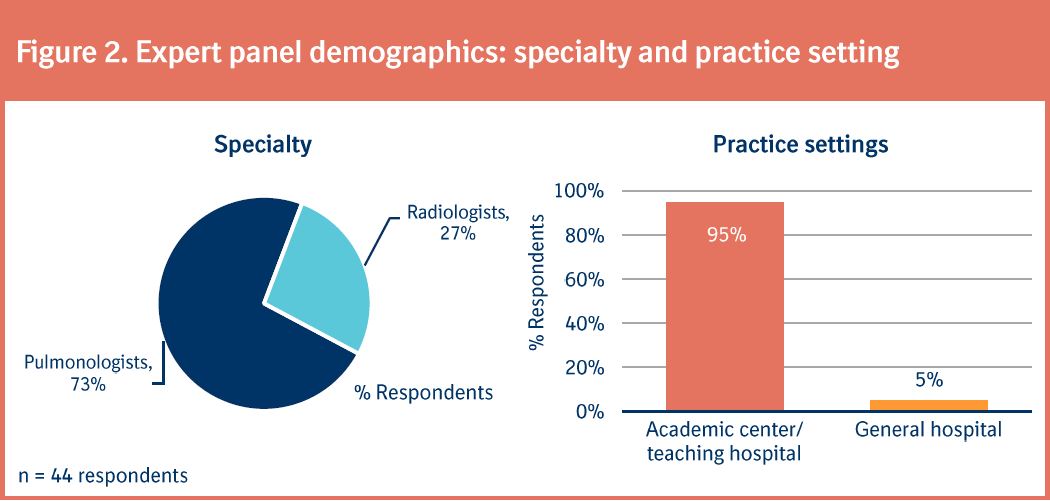
- The expert panel reached consensus that proactive screening for early-stage ILD should be recommended in asymptomatic patients with a history of SSc (Figure 3)
- Consensus was not achieved regarding the need for proactive screening in patients with RA, familial history of pulmonary fibrosis/IIP, or a first-degree relative with pulmonary fibrosis/IIP
Image
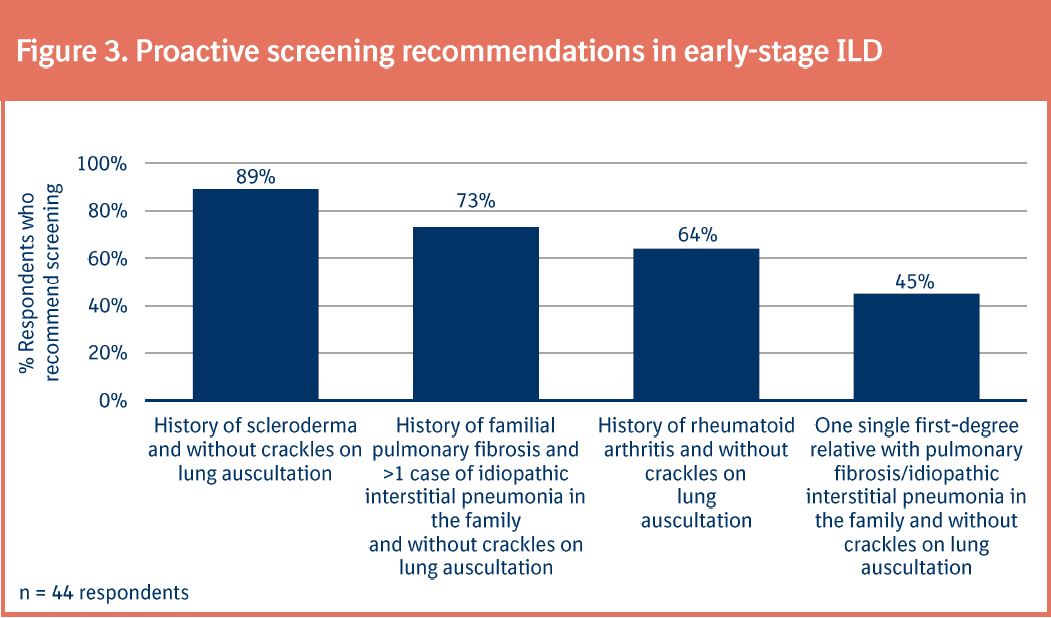
- There was consensus that imaging features of honeycombing indicate the presence of fibrosing ILD (Figure 4)
- Views were divided as to whether traction bronchiectasis was indicative of fibrosing ILD
- Less than half of respondents agreed on whether other ILA, including non-dependent subpleural reticulation and centrilobular ground-glass nodules/patch ground glass opacity, were indicative of ILD
Image
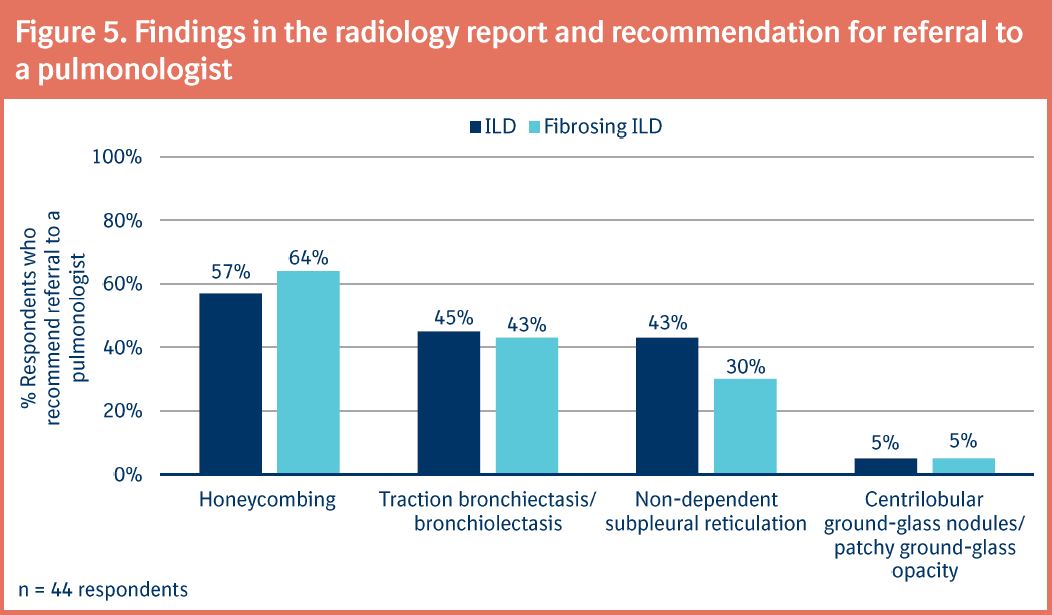
- Although consensus was not reached, most respondents recommended referral to a pulmonologist in patients with honeycombing (Figure 5)
- Under half of respondents recommended referral to a pulmonologist in patients with other listed ILA, including traction bronchiectasis, non-dependent subpleural reticulation or nodules/opacity (Figure 5)
Image
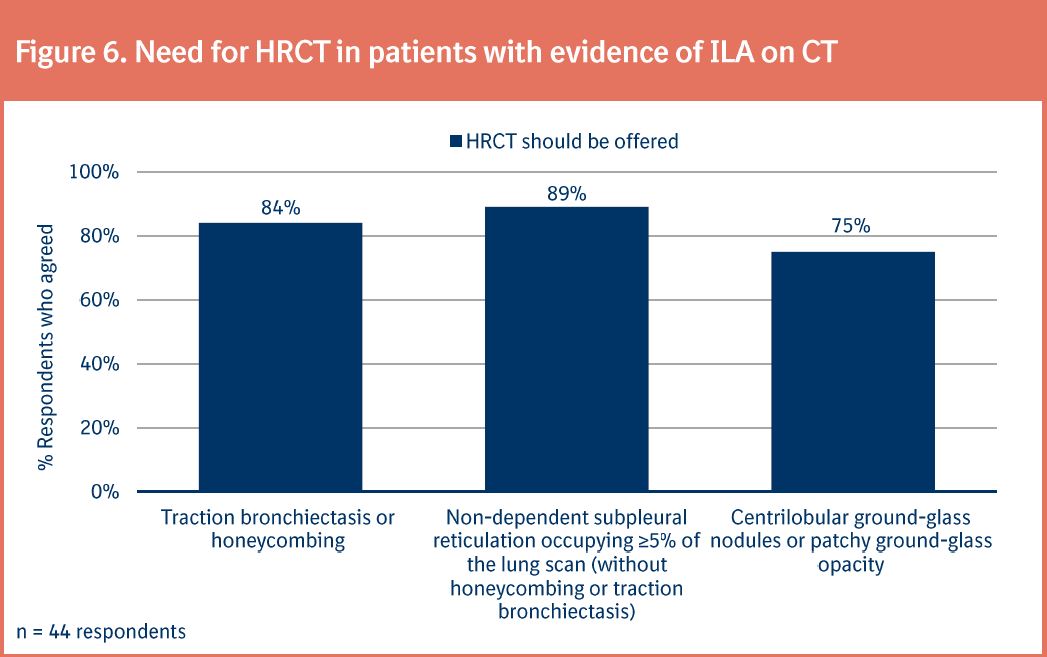
- The expert panel agreed that asymptomatic patients with ILA on CT, including non‑dependent subpleural reticulation, honeycombing/traction bronchiectasis or centrilobular ground-glass nodules/patchy ground-glass opacity, should be assessed further with HRCT (Figure 6)
Image
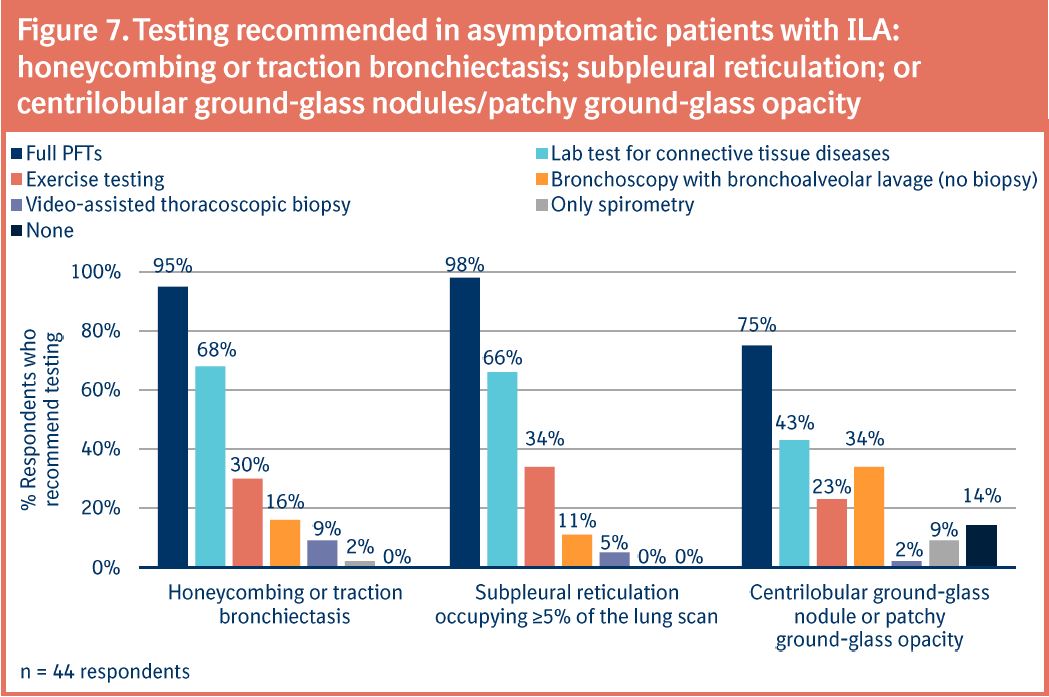
- There was consensus that full PFTs should be ordered when honeycombing/traction bronchiectasis, subpleural reticulation or centrilobular ground-glass nodules/patchy ground-glass opacity are present on HRCT (Figure 7)
- Other tests were less favored
Image
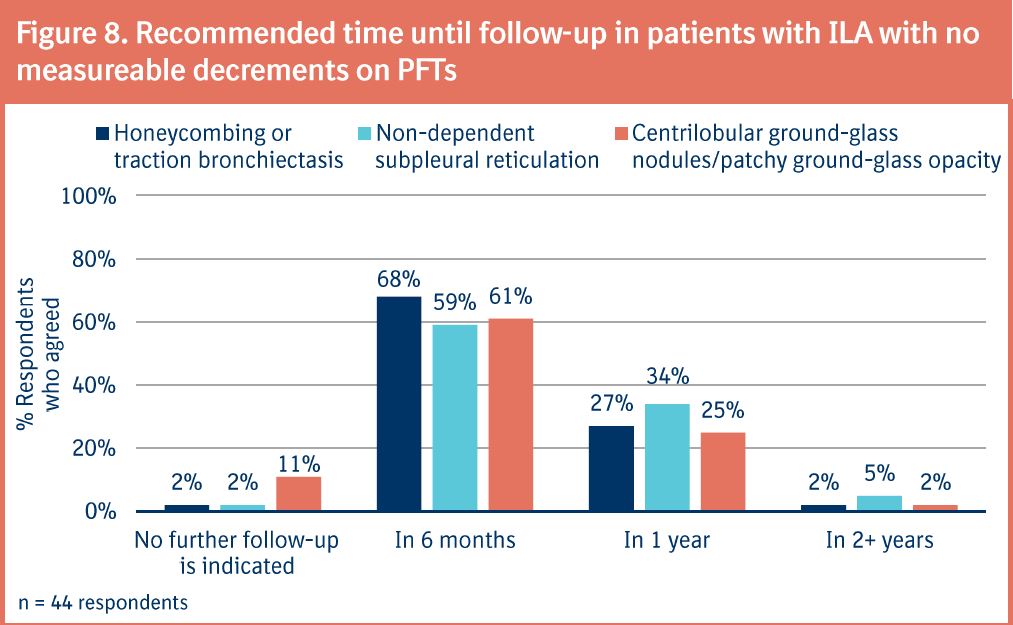
- For all three ILA, >85% of expert panel members recommended that patients should be followed-up within 6‒12 months (Figure 8)
- Consensus was not achieved as to the optimal timing of follow-up evaluation within this range
Image
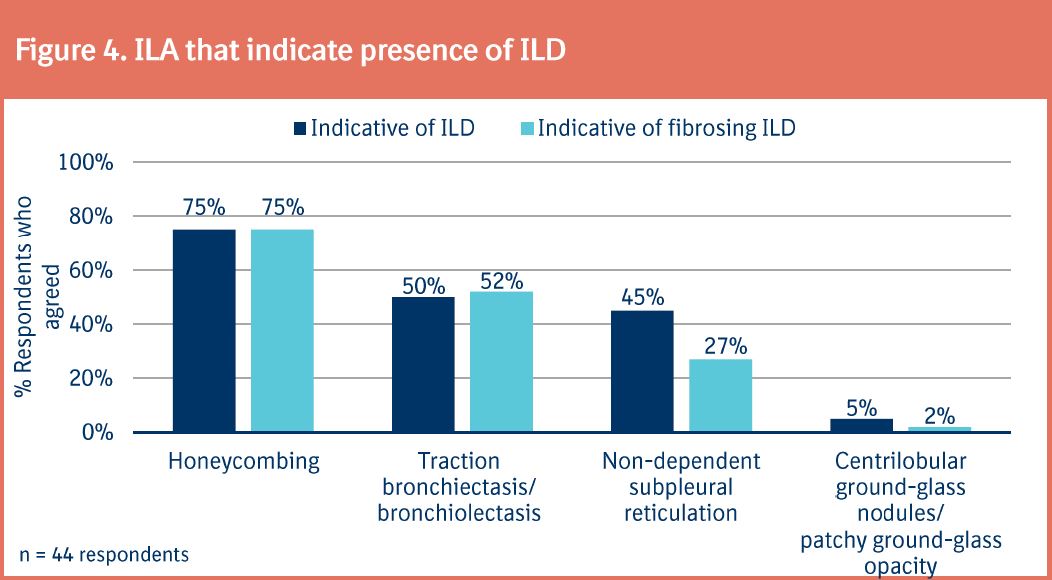
- Consensus was not met regarding the type of follow-up testing required (Figure 9)
- For all three ILA, most expert panel members recommended that patients should undergo full PFTs, but opinions were divided on whether these should be accompanied by HRCT
Image